The Office for National Statistics (ONS) has recently published suicide data by ethnicity in England and Wales (not Scotland) by comparing 2012-2019 death registrations and self-reported ethnicity from the 2011 Census (ONS 2021). Having previously reported only age and gender, this development casts a new light on the UK’s “male suicide crisis” for middle aged and young men (see Samaritans 2012; CALM 2019).
I have argued elsewhere that in light of the UK’s recent and historic immigration practice and policy which produces Britishness as synonymous with whiteness, that the paucity of ethnicity in suicide reporting and thus the prevention campaigns such statistics generate, translates to the male suicide crisis being a crisis for white men (Yue 2021b forthcoming). Like Cohen, Katona and Bhugra (2020), I have called for intersectional suicide reporting which includes ethnicity, in order to better reflect the reality of British people.
Notwithstanding the limits of statistics and their inability to provide a full picture of suicide in the UK, the report is striking. The published figures show that high rates of suicide among men – which have led mainstream suicide prevention charities to generate a “male suicide crisis” – are populated not only by white men but by the suicides of “mixed” men, who the ONS defines as anyone with “multiple ethnic background” (ONS 2021: p.3).[1] What is more, the report finds that suicides are much higher for ethnic minority compared to white women[2]. Female suicide has consistently been swept under the carpet as “failed” attempted suicide (Fullagar and O’Brien 2015).
While the literature on suicide has identified high rates of suicide among ethnic minority and migrant populations (see Forte et al. 2018), these are usually explained away as the result of migrants “bringing” their mental illness with them (see Cochrane and Bal 1987)[3]. And while it is important not to disregard lower rates of suicide among black[4] and other “non-mixed” “non-white” communities, official recording that people with “multiple ethnic backgrounds” (ONS 2021: p.3) are disproportionately dying by suicide is suggestive of a “migrant suicide crisis”. I have written elsewhere (Yue 2021a) about my masters and ongoing PhD research where I look into the ascription of migrant status onto “other” bodies regardless of their being born in the UK or holding British citizenship (see Tudor 2017). Research that second-generation (the children of migrants who are born in the UK and thus have not brought their suicide risk from elsewhere) die by suicide at higher rates than their parents (first-generation migrants) (Forte et al. 2018; Eaton and Harrison 2000) turns the “blame” from individual mental illness to the reality of living in the UK’s “hostile environment” (Fang 2019; The3million.org.uk 2019).
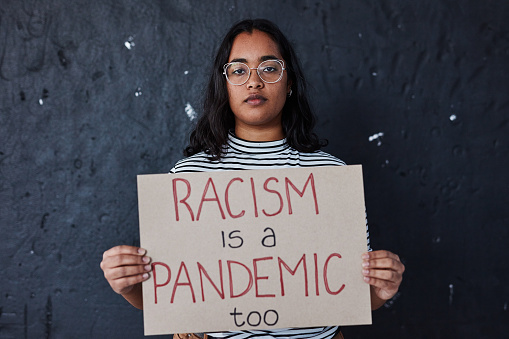
My intention is not to create suicide clusters by evoking a “migrant suicide” crisis[5] but to contend that, if the (white) male suicide crisis has been generated because of high recorded rates of (universal) male suicide, the comparative rates among men who identify as having multiple ethnic backgrounds might mean not only that there is a “migrant suicide crisis”; but that, equivalent high rates of suicide among “mixed” men should generate the same media and policy attention as the plethora of universal male suicide prevention campaigns. As such, race and racism can no longer be absent from them. With the field of suicidology still explicitly (and almost exclusively) valuing quantitative research methods over qualitative (see Hjelmeland 2016), I hope that the ONS’ official publication of ethnicity in suicide statistics will provide an invitation for us to take seriously the effects of racism on the lives (and deaths, including suicides) of ethnic minority people here in the UK.
Bibliography
CALM. (2021). Boys Do Cry – Campaign Against Living Miserably. Retrieved April 8, 2021, from https://www.thecalmzone.net/2017/01/boys-do-cry/?highlight=dont%20bottle
Cochrane, R., & Bal, S. (1987). Migration and schizophrenia: An examination of five hypotheses. Social Psychiatry, 22(4), 181-191.
Cohen, J., Katona, C., & Bhugra, D. (2020). National data on suicide must include ethnicity. BMJ, m4105. doi: 10.1136/bmj.m4105
Eaton, W. and Harrison, G. (2000) ‘Ethnic Disadvantage and Schizophrenia’, Acta Psychiatrica Scandinavica, 102(s407): 38–43.
Fang, N. (2019). Narratively (Bang) Out of Order: On Hostile Environment. International Review of Qualitative Research, 12(4), 385–393. https://doi.org/10.1525/irqr.2019.12.4.385
Forte, A., Trobia, F., Gualtieri, F., Lamis, D. A., Cardamone, G., Giallonardo, V., & Pompili, M. (2018). Suicide risk among immigrants and ethnic minorities: A literature overview. International Journal of Environmental Research and Public Health, 15(7), 1438. doi:10.3390/ijerph15071438.
Fullagar, S., and O’Brien, W. (2015). Speaking of suicide as a gendered problematic. In J. White, I. Marsh, M. J. Kral, & J. Morris (Eds.), Critical Suicidology: Transforming Suicide Research and Prevention for the 21st Century (pp. 94-114). UBC Press.
Hjelmeland, H. (2016). A critical look at current suicide research. In J. White, I. Marsh, M. J. Kral, & J. Morris (Eds.), Critical suicidology. Transforming suicide research and prevention for the 21st century (pp. 31–55). Vancouver, Canada: University of British Columbia Press.
Marsh, I. (2010). Suicide: Foucault, history and truth. Cambridge: Cambridge University Press.
Miklin, S., Mueller, A., Abrutyn, S., & Ordonez, K. (2019). What does it mean to be exposed to suicide?: Suicide exposure, suicide risk, and the importance of meaning-making. Social Science & Medicine, 233, 21-27. doi: 10.1016/j.socscimed.2019.05.019
Moodley, R., Mujtaba, F., and Kleiman, S. (2018). Critical Race Theory in Mental Health. In B. M. Z. Cohen (Ed.), Routledge international handbook of critical mental health. (pp. 15-21). London: Routledge.
Office for National Statistics. (2021). Mortality from leading causes of death by ethnic group, England and Wales – Office for National Statistics. Retrieved 20 August 2021, from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/mortalityfromleadingcausesofdeathbyethnicgroupenglandandwales/2012to2019
Samaritans (2012). Middle-aged men and suicide. Samaritans. Retrieved September 3, 2019, from https://www.samaritans.org/about-samaritans/research-policy/middle-aged-men-suicide/
Sjöström, S. (2018). Labelling theory. In B. M. Z. Cohen (Ed.), Routledge international handbook of critical mental health. (pp. 15-21). London: Routledge.
The3million.org.uk. (2019). The ‘hostile environment’. Retrieved June 27, 2019, from https://www.the3million.org.uk/hostile-environment
Tudor, A. (2017). Queering migration discourse: Differentiating racism and migratism in postcolonial Europe.
Yue, E. (2021a). Migrant Suicide – Suicide Cultures: Reimagining Suicide Research. Retrieved 20 August 2021, from https://blogs.ed.ac.uk/suicide-cultures/2021/03/24/migrant-suicide/
Yue, E. (2021b forthcoming). Migrant Suicide: A Case for Intersectional Suicide Research. Journal Of Ethics In Mental Health, Open Volume(11), 10. Retrieved from https://jemh.ca/issues/open/JEMH-Open-Volume.html
[1] Almost identical at 14.7 deaths per 100,000 males for “mixed” 14.9 deaths per 100,000 deaths for white men (ONS 2021).
[2] “2017 to 2019 there were 7.1 deaths per 100,000 females in the Mixed ethnic group, compared with 4.9 suicides per 100,000 in the White group” (ONS 2021: p.11).
[3] For the past century suicidology has been dominated by understandings of suicide as the result, and evidence of, internal pathology (see Marsh 2010).
[4] For example because of the historical over-diagnosis of their distress (Sjöström 2018), disregard for contextual factors like racism for their distress, and subsequent reluctance to engage with the mental health industry (Moodley et al. 2018).
[5] For the purposes of this blog, I am drawing on Miklin et al. (2019)’s usage of “suicide clusters” that whether exposure to suicide – e.g. via association with those targeted as at risk of suicide in prevention campaigns (see Marsh 2010) – is risky depends on the inferred meaning of the suicide one has been exposed to. In this case, I am arguing that “migrants” are not inherently at risk of suicide, but that racism is productive of suicide, thus turning the potential prevention or “cure” from within the individual – as in suicidology’s compulsory ontology of pathology – to highlighting the affects of, and preventing racism.


Leave a Reply