The Early Years Working Group, together with Better Births Initiative (Royal College of Midwives) and the Evidence for Action Team (NHS Health Scotland) recently organised a free, half-day event at the University of Edinburgh to promote effective continuity and transition of care throughout maternity and to health visiting services. The event brought together about thirty-five participants from midwifery, health visiting, academia, policy and the voluntary sector working across the UK.
As part of the programme, participants initially identified the key barriers to continuity and transition of care in practice. They were then given opportunity to hear from four different speakers. Dr Mary Ross-Davie (NHS Education for Scotland) gave an overview of the research evidence for continuity of carer. Professor Mary Renfrew (University of Dundee) talked about continuity of care in midwifery and its contribution to quality of care of women and newborn infants. Wendy Mitchell (NHS Lanarkshire) then presented on continuity and seamless transition of care from midwifery to health visitor, focussing on child protection. Finally, Ann Holmes (Scottish Government) spoke about the Scottish policy context of continuity and transition of care.
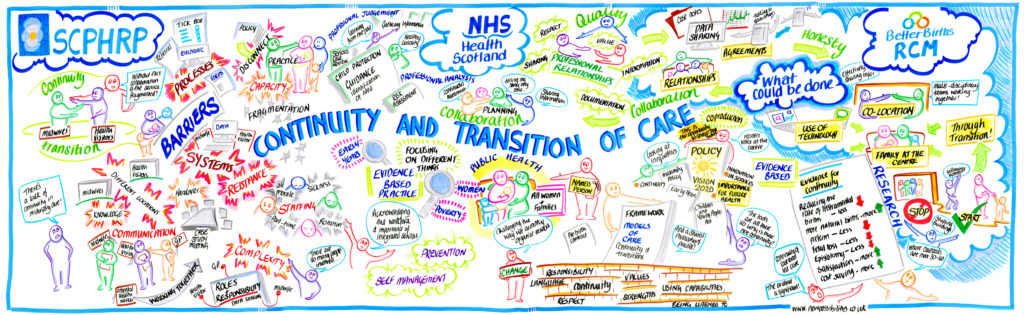
At this stage, participants discussed the proceedings of the day and identified ways in which continuity and transition of care could be further improved both within and between midwifery and health visiting services. The conversations of the day were captured by our brilliantly creative Graphic Recorder Anna Geyer.
Summary
The following were practitioners’ views on barriers and facilitators
- Systems and processes where practitioners are not sharing information and are not sure what was appropriate to share or not
- Interruptions to continuity from a staffing perspective was mentioned such as part-time working, rotations, and sickness affecting presence
- Disconnect between the policy statements and the practice capacity affecting the change that can happen
- Co-location was seen as an enabler and the benefits of being in one building and have mini case conference and other contacts
- There was a need to differentiate the responsibility towards the child rather than the family in the context of child protection. Sometimes the relationship needs to be interrupted for providing quality of care with referrals etc.
- Having the family at the centre of care such as bringing the clinics to the people based on their timings and at convenient locations (attractiveness of locations for accessing care) for midwifery
- Achieving quality through the building of professional relationships and collaborative working, having respect for each other’s roles and contributions, and auditing the communications
What’s next?
Another event will be planned for Autumn 2016 and will focus on the early years and health visiting.