On Monday 28th November, ECRED held its first in-person event since the pandemic. The event rekindled old connections, enabled new connections to form, and provided a space for collaboration and reflection.
The event began with a beautiful moment of connection facilitated through guided meditation exercises led by Dr Gill Matthews and Martha Pollard. We then worked collaboratively in groups on a collective response to the Scottish Government’s call for input into their new dementia strategy, followed by watching a new film on the value of counselling for those living with dementia. Lived experience researcher Martin Roberston and Dr Gill Matthews facilitated a feedback session on the film, inviting questions and reflections on how to use the film to advocate for counselling models in dementia care.
Finally, we engaged in a group singing activity led by PhD researcher Lucy Forde, energising us as we entered informal networking after the event.
We wanted to take this opportunity to share with you the written outcome of our collective response to the Scottish Government’s call for input into their new dementia strategy. Questions were provided to us which we answered together, with the responses now submitted to the government. Here’s what we said:
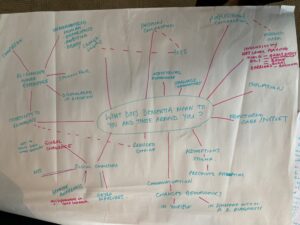
1. What does dementia mean to you and those around you? The word ‘dementia’ often comes with stigma and fear, and the language connected to it can be misunderstood. Dementia affects people in different ways, with some experiencing a sense of loss and isolation, as well as fractured care and support. Many living with dementia and their unpaid carers experience mental health challenges and these are not talked about. We believe there needs to be greater awareness of dementia that will enable an opportunity to re-imagine what it means to be human. This re-imagining needs to see those with dementia as ‘whole’ people that have something to offer to society – with potential – and facilitate compassion. We need to challenge assumptions of what people living with dementia are capable of, providing opportunities for growth and flourishing with a diagnosis. The pandemic has shown us that people can adapt when they have to, and we need to provide the societal structures necessary to create an environment for society to change their attitudes towards those living with dementia – we need radical social change. As part of this, we also need to see a consistent national approach and have a multi-skilled workforce who are trained in working with those at all stages of living with dementia, including knowledge of the anticipatory grieving process for both carer and those living with a dementia diagnosis.
2. What supports work well for you? We feel that this question suggests that there are available supports that work well, but there is a lack of support and a lot that could be improved. For example, post-diagnostic support does not support everyone. When it came in, it did not include those in later stages of dementia who had previously had a diagnosis. For those in later stages, they have felt ‘abandoned’ and ‘left to rot’ by the government. Further, despite previous policy strategies, there is still lack of education around what supports are required for those living with dementia (and how they can be individualised and personalised to meet individual needs), as well as a lack of support. Support is also not always accessible, and there needs to be a more consistent and standardised strategy that enables all those who need support to access it. This access should be when those living with dementia need it, rather than at a prescribed time (e.g., at diagnosis) or for a limited period. We have also found that counselling for those living with dementia does provide important psychological support, but it is not widely offered and more funding is needed to provide sustainable and accessible counselling models.
3. What challenges need to be addressed? Someone living with dementia in our community who was diagnosed last century shared that when he heard the words ‘you have dementia’, he was told that he had up to 6 years to live and told to come home and put his affairs in order – he did not experience any post-diagnostic support. Others in our community have also explained that even now, many years on, there is a lack of information at the time of diagnosis and receiving support is ‘a postcode lottery’. This person living with dementia also explained how his family knew nothing about dealing with dementia and that ‘it was the most terrifying episode in our lives’ which could have easily broken up the family due to the challenges of living with dementia. Many living with dementia do experience broken families as a result, and more needs to be done to change the stigma of having dementia, ensuring that support is provided to those with a diagnosis and to families and friends. There is a sense that those with more advanced dementia have ‘had their day’, and we need to work to change this to show the value that those with dementia can add to communities. A major issue is also funding. There are community supports that can provide opportunities for those with dementia to be active citizens, such as engagement in the arts and creativity, or becoming involved in coproduced research or policy, but more money is needed to provide the structures required to deliver these programmes equitably and sustainably. In view of Covid-19, many community opportunities have also been reduced, resulting in increased isolation. The realities of the post-Covid landscape need to be addressed.
4. How would addressing these challenges change lives? We feel that the 1-year of support offered as part of post-diagnostic support should be from when you need it, not from a formal diagnosis, as the diagnosis process can take a long time. Many need support ahead of their diagnosis. Further, we feel that longer than 1-year is needed. This would provide early support that could prevent major psychosocial problems experienced when coming to terms with a dementia diagnosis. Annual reviews also often don’t happen at the GP when they should, and they need to happen. Addressing this would provide the respect and dignity that those living with dementia should receive, ensuring ongoing support and being there for every part of living with dementia. Many people living with dementia also experience mental health challenges and there is an urgent need for psychological support to be more widely available (such as counselling and creative arts therapies) and for healthcare staff to be trained in supporting the mental health of those living with dementia. A better understanding of peer-to-peer support is needed as this can mean many things, along with better access to digital communities for rural communities. We also need individualised, personal care that acknowledges individual needs and preferences, as well as strong community support and care. In relation to the latter, this should include access to creative and cultural engagement. Individualised and community care can support to improve wellbeing, quality of life, and flourishing, enabling those with dementia to live well and contribute actively to our communities. In relation to community initiatives and peer support, we also need a better understanding and investigation of social return on investment, understanding how much money these initiatives may save in the long run for our health and social care services. We also feel that IT/digital technologies and creative engagement can support with keeping those living with dementia active, thereby supporting both physical fitness and psychological health.
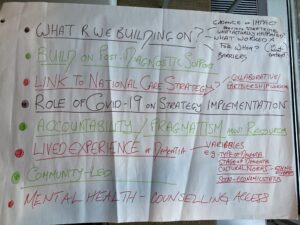
5. What do we need to build on/learn from what has been done before? We would like to know more about the impact of the previous dementia strategy – who did it work for and what were the barriers? We also feel that we should be building on the post-diagnostic support that is currently offered, ensuring it reaches those who need it as early as possible and can be sustained into the later stages of living with dementia. We feel that there is a need for better collaboration across policy bodies too. In this post-pandemic time, resources and time are limited and if we can work together, it will strengthen our infrastructure and we can be more ambitious with what we can achieve. This could be, for example, working with those in cultural policy as part of community asset-based and arts on prescription schemes. We would also like to know more about the impact and role of COVID-19 and how this may have affected policies from the previous strategy. We feel that many ambitions from the previous strategy have not been practically achieved and that more needs to be done to action policies and provide funding to achieve positive change for our dementia communities. This should also include a close analysis of who may be missing from policies because of structural inequalities (e.g., based on socioeconomic status, ethnicity, stage of dementia). We need to ask: How do we ensure all voices are heard?
Thank you to everyone who came to our networking event, and we hope to see you again next time! If you’re new to ECRED and interested in attending an event with us in the future, please contact ecred@ed.ac.uk