The Lancet Commission On Global Surgery
Surgeons have long felt that the importance of surgery has been lost in past efforts to impact on global health issues. The Lancet Commission on Global Surgery seeks to address deficiencies in surgical and anaesthetic care, provide evidence and solutions for achieving health, as well as welfare and economic development through the strengthening of surgical health systems in Low and Middle income Countries (LMIC).
Twenty five commissioners have worked for almost 2 years consulting extensively in over 100 countries in 6 continents. Their report may not please all but is a significant achievement. Surveys, epidemiological studies, estimates, audits and mapping programmes helped to provide evidence and to highlight further disparities in surgical care through 5 key messages at their recent London and Boston launches:
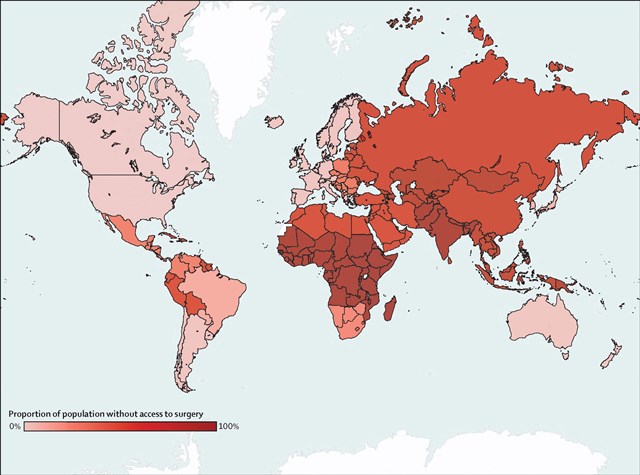
- 5 billion people lack access to safe affordable surgical services when needed. Nine of ten people in low-income and lower-middle-income countries cannot access basic surgical care.
- 143 million additional surgical procedures are needed each year to save lives and prevent disability. Only 6% of 313 million procedures that are undertaken worldwide annually, are performed in the poorest countries.
- 33 million individuals face catastrophic health expenditure to pay for surgical services.
- Investment in surgical and anaesthetic services saves lives, is affordable and promotes economic growth.
- Surgery is an indispensible part of health care and should be an integral component of a national health system in countries at all levels of development.
The Lancet, DOI: 10.1016/S0140-6736(15)60160-X, Copyright @ 2015 Elsevier
The Commission’s stated targets for 2030 are daunting:
- A minimum of 80% coverage of essential surgical and anaesthesia services per country.
- 100% of countries with at least 20 surgical, anaesthetic, and obstetric physicians, per 100,000 population.
- 100% of countries tracking surgical volume, a minimum of 5000 procedures per 100,000 population.
- 100% of countries tracking perioperative mortality.
- 100% protection against impoverishment from out of pocket payments for surgical care.
- 100% protection against catastrophic expenditure from out of pocket payments for surgical care.
Some might see these as challenging for some developed countries so how can these objectives be met in developing countries where increasing funding of health care still results in disparities.
We know that targeting specific health care issues through philanthropic support in the developing world has brought about mixed success. Numerous philanthropists and charities have stumbled in attempting to deliver sustainable solutions when investing in facility or service. Outreach programmes from well intended overseas surgical teams may actually impact adversely on the very environment that they hope to support. Essential emergency provision of surgical care may be compromised when, for example, limited facility is set aside for the orchestrated elective missionary surgery. The conditions or surgical pathology targeted or technology being shared may seem entirely appropriate to the visiting team but may be largely irrelevant to the needs of the local population.
Investment in infrastructure may seem to produce a tangible legacy for the donor but it is challenging to maintain such quality facilities when these are seen by some as a source of material to be plundered to support their families in desperate financial need. Furthermore, some initiatives have been been criticized for focusing too narrowly on the capacity of science and in neglecting the importance of economic, social, and political factors. Such surgical initiatives require significant funding and need to be considered in parallel with improvements in public health, education and the health system. Pressurised surgical services dealing with trauma in the developing world might rather welcome greater health and safety regulation, improvements in street lighting, better maintained roads and greater driver regulation.
So where to start? Records often do not exist so reliable surgical audits or death rate statistics for surgery do not exist in LMIC. Investment in information technology is limited in most developing countries but finance is required to obtain key information that would identify clearly the needs of surgical services in the LMIC. GlobalSurg is a collaboration supported by Clinical Surgery at the University of Edinburgh (http://globalsurg.org/get-involved/). The group is currently using an international network of training and qualified surgeons to study variation in outcome of emergency intra-abdominal surgery across various clinical settings. It will determine whether globally relevant quality improvement strategies are needed within acute surgical units. This project would serve to provide much needed information in an area of acute surgical care and will allow development of regional, national and international surgical networks. The group recently published on the benefits of these networks in the Lancet. There is no reason why the group cannot establish key global studies, including the opportunity for randomised trials.
The Lancet, DOI: 10.1016/S0140-6736(15)60160-X, Copyright @ 2015 Elsevier
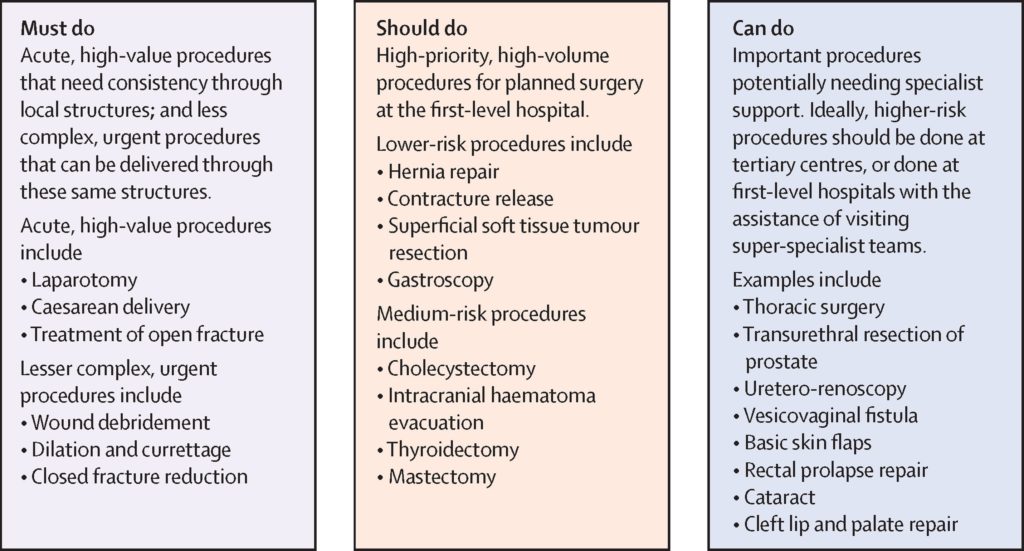
Humanitarian and global surgical outreach programmes have been supported by surgical colleagues in Edinburgh at considerable personal social and psychological sacrifice. Such direct support has undoubtedly had significant impact on the lives of those affected by conditions including those arising from complications of obstructed labour. The social stigmata attached to this condition are considerable and the repair transforms the patient’s existence. And yet, the procedure to correct a vesicovaginal fistula is categorized as a ‘can do’ rather than a ‘must do’ surgical procedure. Where should the priorities lie when the challenge is so immense? How can such outreach programmes deliver a legacy in a developing country?
The target set by the Commission that 100% of countries should have at least 20 surgical, anaesthetic, and obstetric physicians per 100,000 population is formidable. We have experience supporting surgical training in Malawi which produces some 100 medical graduates per year. However, for a population of 17 million people, there are currently only some 15 trained surgeons in practice since many move overseas when they are exposed to the opportunities that exist for well-trained doctors in the developed world. The Lancet Commission requirement by 2030 is projected at 60 specialists per 100,000 population. It is difficult to imagine where the additional 10,000 or so specialists will emerge for Malawi without substantial investment.
Scotland has a strong tradition of investing in education on Africa. Gordon Brown as UN Special Envoy for Global Education, and through the Office of Gordon and Sarah Brown, has promoted and initiated education programmes in Africa. Edinburgh University has invested strongly in postgraduate educational initiatives that have benefited LMIC. The huge success of our own surgical distance learning programmes has allowed us to support more trainees from these countries.
Our surgical Masters programmes currently have over 450 students enrolled in 40 different countries. In 2009, the Scottish Government and J&J/Ethicon supported the University of Edinburgh and the Royal College of Surgeons of Edinburgh to deliver free postgraduate educational support to training surgeons in Malawi. Since then, the first three students have graduated from the three-year distance learning course which supports the educational and professional needs of the young training surgeon. Six more Malawian trainees are currently in the programme. Surgical trainees have been supported without the need to remove them from the area of greatest need. The programme content adds value to their in-the-workplace training and allows the young surgeon to attend to local service needs. We are also aware that educational resource has been extended to medical assistant practitioners who are a vital link in the surgical care chain.
The Lancet Global Commission has ensured that surgery can no longer be overlooked as a health need for the world’s poorest people. The Commission has set itself ambitious targets but no one initiative will address the current unmet need. Better global surgical and anaesthesia care will only be realised through increased investment in human and physical resources. Early and urgent domestic and external investment in surgical and anaesthesia care is needed to realise these returns. Our group sees itself as being in a strong position to invest in the postgraduate education of the surgical workforce in these countries.
Similarly, research, monitoring, and assessment will have to play an increasing and crucial part in the future of global surgical and anaesthesia care. There is a paucity of scientific rigor around implementation science, and an absence of globally accepted surgical metrics which have contributed to past neglect of surgical and anaesthesia care within global health. A commitment to better understand the problems and solutions should be a priority for those dedicated to improvement of surgical and anaesthesia care worldwide. We will continue to invest primarily in the training surgeons in these LMIC through postgraduate education. In this way, we should empower the very body that can engineer change locally so that we might yet see some practical light at the end of a very long tunnel.
Professor O James Garden, Regius Professor of Clinical Surgery and Honorary Consultant Surgeon, University of Edinburgh